Pending Claims Management (Revenue Cycle Management)
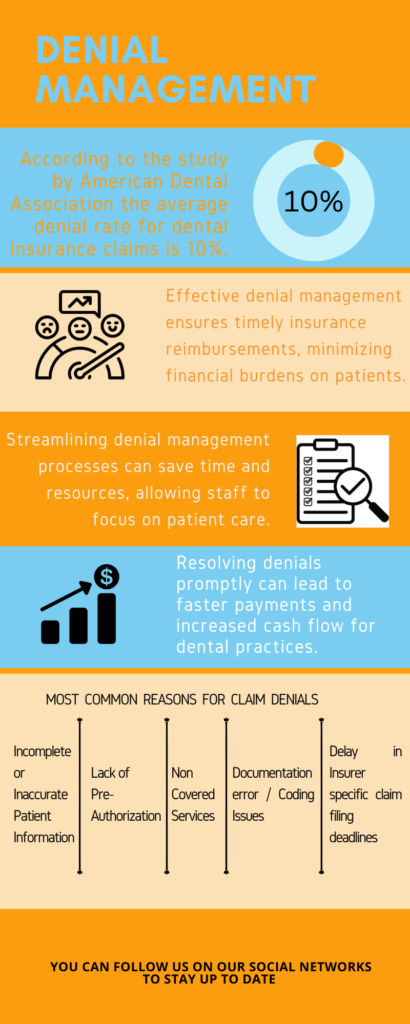
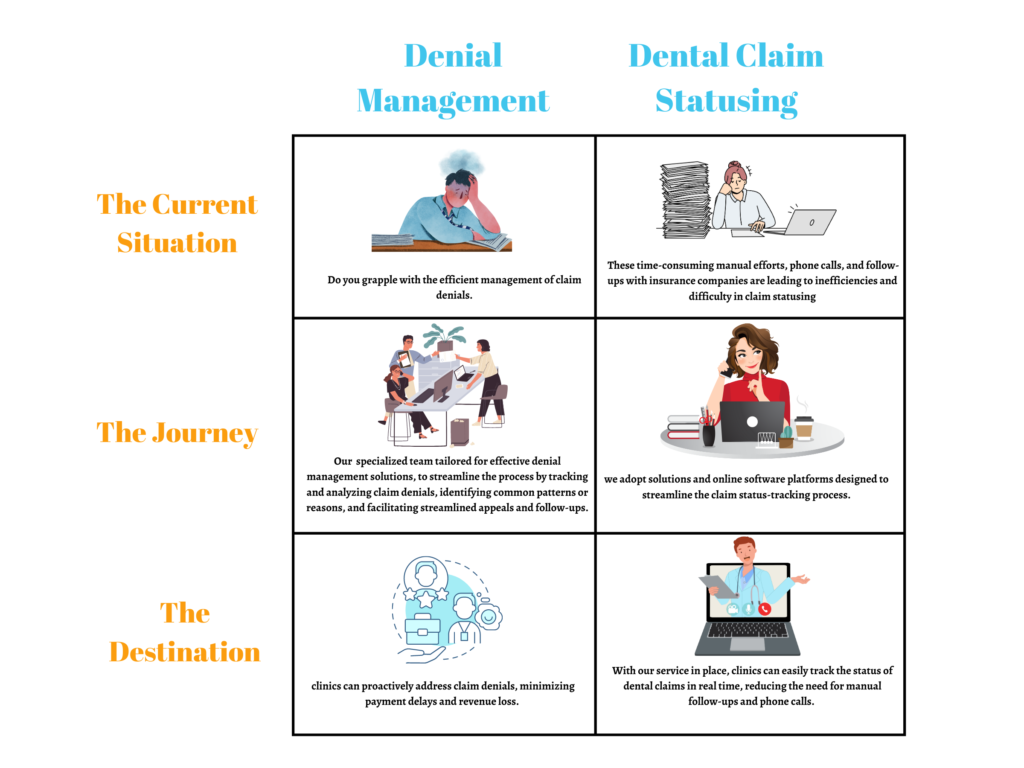
Navigating insurance denials can be a challenging and time-consuming process for dental practices. Understanding the reasons behind denials, appealing claims, and recovering lost revenue requires expertise and dedicated resources. Our denial management services are designed to streamline this process and help you overcome insurance roadblocks effortlessly. Our experienced team meticulously analyzes denials, identifies patterns, and develops effective strategies to maximize claim acceptance. We handle the time-consuming tasks of claim resubmissions, appeals, and follow-ups, allowing your staff to focus on patient care.
By leveraging our denial management services, you can minimize revenue loss, reduce administrative burdens, and improve overall practice efficiency. Let us help you navigate the complexities of insurance denials, ensuring you receive the rightful reimbursement you deserve.
Pricing
- Basic
- $ 1.75/claim
- Dental Claims Statusing
- (30 to 119 days)
- Contact Now
- Silver
- $ 2.25/claim
- Dental Claims Statusing
- (30 to 119 days)
- Denial Management(Adjustments, moving balances to patient and Electroni Resubmission)
- Contact Now
- Gold
- $ 2.25/claim
- Dental Claims Statusing
- 120 days or older upon the commencement date of service
- with or without Denial Management(Adjustments, moving balances to patient and Electroni Resubmission)
- Contact Now
Schedule a Meeting with our Team
Total Number of Hrs employee works =
Avg Cost for Indian Employee =
Avg Cost for Foreign Employee =
Brochure
Case Study
White Paper
Elevate your business with our comprehensive white paper, meticulously crafted to provide an in-depth understanding of how our services can revolutionize your operations. Explore its concise yet impactful content to make informed decisions and drive sustainable growth.
Solo Dentist – Increase your reimbursement rate
Denial Management – Effective denial management is crucial for solo dentists to ensure smooth revenue cycle management and maximize reimbursement for their dental services. By implementing robust denial management processes, solo dentists can efficiently handle claim denials, identify root causes, and take appropriate actions to resolve and resubmit claims. This proactive approach helps minimize revenue loss, streamline administrative tasks, and maintain financial stability for the dental practice.
Dental Claim Statusing –
Dental claim statusing is a vital process for solo dentists to track the progress and status of submitted claims. By actively monitoring claim status, solo dentists can ensure timely reimbursement for their services, identify potential issues or delays, and take appropriate actions to resolve any outstanding claims. This proactive approach helps maintain a healthy cash flow, improves practice efficiency, and enhances overall revenue cycle management.
Regional Group – Improve consistency across your group practices
Denial Management – Denial management holds significant importance for mid-sized dental practices. By implementing structured denial management strategies, these practices can effectively handle claim denials, reduce payment delays, and optimize revenue generation. Proactive identification of denial patterns, effective communication with payers, and timely appeals contribute to improving cash flow and maintaining strong financial performance for the practice.
Dental Claim Statusing –
Dental claim statusing holds significant importance for mid-sized dental practices. By implementing efficient claim statusing processes, these practices can closely monitor the progress of submitted claims, identify denials or delays, and address any outstanding issues promptly. Proactive follow-up on claim status allows mid-sized practices to optimize revenue collection, minimize payment delays, and ensure smooth cash flow management.
National Group – Get intelligence to monitor and streamline calls across Nation
Denial Management – Denial management is a critical component of revenue cycle management for large Dental Service Organizations (DSOs). By leveraging denial management tools and dedicated resources, DSOs can efficiently handle claim denials, track denial trends across multiple locations, and implement corrective measures. Proactive denial prevention strategies, continuous process improvement, and effective collaboration with payers contribute to optimizing revenue and ensuring financial stability across the organization.
Dental Claim Statusing –
Dental claim statusing is a critical aspect of revenue cycle management for large Dental Service Organizations (DSOs). With a high volume of claims across multiple locations, effective claim statusing enables DSOs to closely track and manage the status of submitted claims. Proactive monitoring, timely follow-up, and efficient resolution of claim issues contribute to maximizing reimbursement, improving financial performance, and streamlining revenue cycle operations within the organization.
Services Offered by Todays Dental Partners
 |
Denial ManagementDenial management tackles insurance claim denials in the dental industry. It involves identifying denial reasons, minimizing rejections, and managing appeals. Streamlining denial management optimizes revenue, reduces administrative burden, and ensures prompt reimbursement. Focus on quality care while we handle denials efficiently. |
 |
Dental Claim StatusingDental claim statusing involves tracking the progress of insurance claims. Key meanings include: “Submitted” (claim sent), “Received” (acknowledged), “In Review” (under evaluation), “Pending Additional Information” (require more documentation), “Adjudication” (calculating payment), “Denied” (rejected), “Approved” (accepted), and “Paid” (processed and paid). Understanding these statuses helps dental providers stay updated on claim progress for efficient processing and reimbursement. |
Our Timeline
Day 1
“Our team will provide you with a letter of engagement, offering comprehensive denial management and claim statusing services. We specialize in efficiently and accurately handling the resolution of claim denials and providing timely updates on the status of your claims. With our expertise in the field, we ensure effective management of denials and claim processing.”
Day 7
“We will dedicate up to a week to thoroughly understand your denial and claim statusing processes. This includes reviewing relevant documents and understanding your practice’s unique requirements. By doing so, we can effectively and promptly manage denials and provide timely updates on the status of your claims without any errors.”
Day 7-30
“We will establish targets for the number of denials to be resolved and claims to be accurately updated on a regular basis. Our goal is to manage denials efficiently and accurately, ensuring timely resolution and providing up-to-date information on the status of your claims.”
Day 30
“Denial management and claim statusing is an ongoing and iterative process. To maintain accurate records, we conduct monthly assessments to ensure error-free reports. At the end of each month, we will provide you with an analysis report of your practice’s denial management activities and claim status updates.”
Day 60
“By outsourcing your denial management and claim statusing tasks to us, you can expect clean and organized records. Your front office staff will have sufficient time to focus on their core responsibilities, while dentists can prioritize delivering excellent patient care. By entrusting us with your denial management and claim statusing, your practice can save valuable time and resources.”
Testimonials
 |
 |
 |
| Dr.Emily Johnson | Dr.Mark Davis | Dr.Sarah Collins, |
| Johnson Dental Care | Healthy Smiles Dentistry | Smile Dental Center |
| ” The dental claim statusing services provided by Todays Dental Partners have been exceptional. Their efficient tracking system keeps us updated on the progress of our claims. We appreciate their prompt and accurate status updates, which have improved our practice’s workflow and reduced administrative hassle. A reliable partner indeed!” | “We were struggling with managing insurance denials until we partnered with Todays Dental Partners. Their denial management services have transformed our practice. They expertly handle appeals, streamline the process, and have improved our cash flow. Thanks to their support, we can now focus on patient care with confidence.” | ” Todays Dental Partners helped our Office to get the proper Claim Management system. They have a workflow on the process which worked for our clinic really well. |
FAQs (Frequently Asked Questions)
What is denial management in the dental industry?
Denial management refers to the process of identifying, analyzing, and appealing denied insurance claims in dental practices. It involves addressing the reasons behind claim denials and taking proactive measures to optimize reimbursement and minimize revenue leakage.
Why do dental claims get denied?
Dental claims can be denied for various reasons, including inaccurate or incomplete documentation, coding errors, lack of medical necessity, eligibility and coverage issues, and contractual or compliance issues. Understanding the causes helps in implementing effective denial management strategies.
How does denial management impact dental practice financially?
Denials can have a significant financial impact on dental practices. They lead to revenue leakage, decreased cash flow, and increased administrative costs. Effective denial management helps identify and address issues, ensuring accurate reimbursement and financial stability.
How can denial management improve the efficiency of practice?
By implementing denial management strategies, you can streamline workflows, reduce administrative burdens, and enhance efficiency. This allows your staff to focus more on patient care and reduces the time spent on appealing denied claims.
Can denial management help with compliance and regulatory requirements?
Yes, denial management processes help ensure compliance with payer guidelines and regulatory requirements. By identifying and rectifying compliance issues, you can minimize the risk of penalties and reputational damage to your practice.
What are some best practices for effective denial management?
Best practices include accurate and complete documentation, robust coding and billing processes, verification of eligibility and coverage, root cause analysis of denials, streamlined appeal processes, and leveraging technology solutions such as denial management software.